Impact of Physical Therapy in Reducing Falls and Fall-Related Costs
Falls, often perceived as mere accidents, are a significant and rising concern. Shockingly, someone experiences a fall every second around the globe and one in four adults fall every year. These incidents, whether due to tripping on uneven surfaces, slipping on wet floors, or health conditions like osteoporosis and Parkinson's disease, are multifaceted in their causes.
The aftermath, however, is profound, leading to both immediate and ongoing injuries and surging financial implications for health plans and provider groups. Alarmingly, the costs related to falls in the U.S. are projected to rocket from $50 billion to $70 billion annually in this decade.
Why are Falls So Expensive
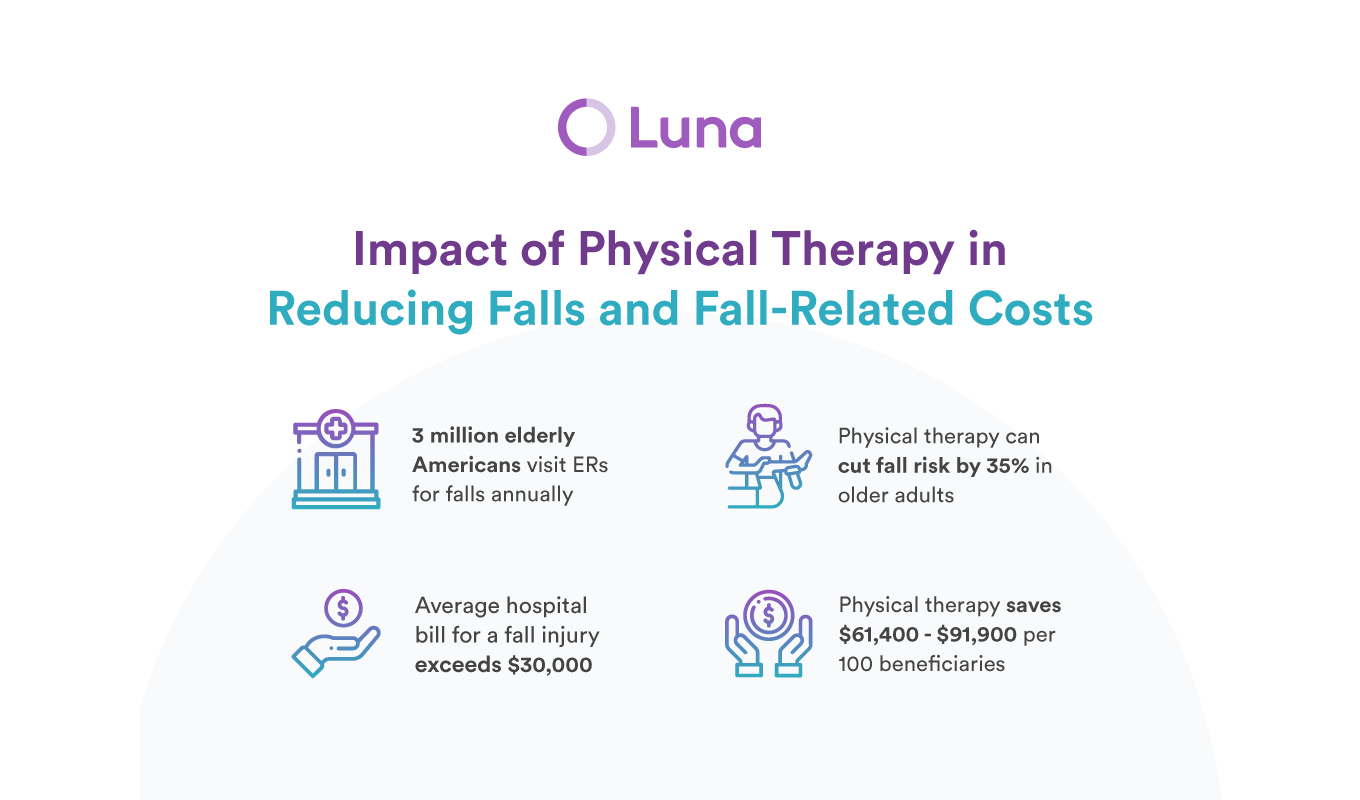
Annually, 3 million elderly individuals across the United States receive treatment in emergency rooms due to falls, with over 800,000 leading to hospitalization (27%), predominantly from head injuries or hip fractures. Notably, falls account for the vast majority of hip fractures and stand as the leading cause of traumatic brain injuries.
In fact, one in every five of these falls results in grave injuries like broken bones or head injuries. Significantly, more than 95% of hip fractures are a direct result of falls, typically from falling sideways. Falls also stand out as the leading cause of traumatic brain injuries. And unfortunately, falling once doubles your chances of falling again.
The financial toll is substantial: hospital costs account for more than half of the total spending on fall injuries, and the average hospital bill for a fall injury surpasses $30,000. The expense can fluctuate based on the severity of the injury and the length of the hospital stay.
Physical Therapy: A Dual-Faceted Approach to Fall Management
Physical therapy (PT) not only plays a pivotal role in post-fall interventions but also stands out as a preventive measure, tackling the issue before it arises.
Prevention Before the Fall
Several studies accentuate the preventive potential of PT in mitigating the risk of falls. The Otago Exercise Program, an eminent strength and balance exercise regimen, has garnered significant attention in this regard. With its rigorous research backing, this program has shown a remarkable reduction in falls by 35% among community-dwelling older adults. Similarly, a 2019 Cochrane review brought to light the efficacy of exercise programs in preventing falls. It elucidated that such programs curtailed the rate of falls by 23% and decreased the risk of individuals experiencing one or more falls by 15%. The exercises do not require special equipment and can all be completed at home.
It's essential to note that the success of these exercises often hinges on consistent adherence. This is where PT shines: having a therapist guide ensures commitment and an ongoing adoption of these regimes. Plus, therapists possess the expertise to craft the optimal mix of exercises tailored to an individual's needs, ensuring greater success.
Post-Fall Recovery
A study, commissioned by the Alliance for Physical Therapy Quality and Innovation, underscored the benefits of PT in the aftermath of falls. Medicare patients who pursued PT post-fall saw a staggering 50% decrease in emergency room visits or hospital admissions within the ensuing six months. This reduction trend persisted even 7-18 months after the fall. For every 100 beneficiaries utilizing PT after a fall, there are savings ranging from $61,400 to $91,900.
Moreover, those who underwent more than 30 PT sessions exhibited the lowest odds of subsequent ER visits and hospitalizations.
Furthermore, post-fall PT also correlated with a 39% reduction in opioid consumption over the subsequent six months. Given the overarching concerns about opioid dependency, this is a significant factor for health plans to consider.
How PT Mitigates Fall Risks
The preventive and reactive strategies of PT encompass:
- Muscle strengthening to tackle weak leg muscles, a primary fall risk.
- Balance Training to address postural instability.
- Gait Analysis and Training to correct irregular walking patterns.
- Functional Training for practical day-to-day activities.
- Environmental Modifications to ensure safer living spaces.
- Exercises definition and adoption to ensure correct compliance with exercise programs.
- Education on fall risks and preventive strategies.
- Assistive Device Training to teach the correct use of aids like canes or walkers.
- Vestibular Rehabilitation for those with inner ear issues.
- Joint Mobility Enhancement to address gait and balance issues.
Future Outlook: Bridging Reactive and Proactive Strategies
As health plans and providers contemplate PT's role, not just as a post-fall intervention but as a preventive strategy, the road ahead seems promising. And while falls might seem unintentional, their management need not be merely reactive. Physical therapy provides a proactive, cost-effective, and patient-focused solution, promising tangible dividends for health plans and provider groups. As the healthcare realm evolves, placing PT at the forefront of fall management is not just beneficial - it's essential.
References:
- Desmarais, M., Kalidindi, Y., & Kramer, R. (2023). Impact of Physical Therapy on Opioid Use and Hospitalizations Post-Fall in Medicare FFS Patients. Alliance for Physical Therapy Quality and Innovation Memorandum.
- Data Source: 2016-2019 100% FFS Medicare Claims Data.
- CDC. (2020). Important Facts about Falls. https://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html and https://www.cdc.gov/falls/facts.html
- World Health Organization. Falls. https://www.who.int/news-room/fact-sheets/detail/fall
- CDC. (2016). Costs of Falls Among Older Adults. https://www.cdc.gov/homeandrecreationalsafety/falls/fallcost.html
- CDC. (2017). STEADI - Older Adult Fall Prevention. https://www.cdc.gov/steadi/index.html
- Otago Exercise Program, UNC website. https://www.med.unc.edu/aging/cgwep/courses/otago-exercise-program/
- Cochrane, Preventing falls and fall-related injuries. (2018). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6360922/
This entry was posted in Luna Blog and tagged Patients, Health Plans.


